Health &
Wellness Blog
Articles and resources to help you stay your best from your therapists at ProTouch Physical Therapy
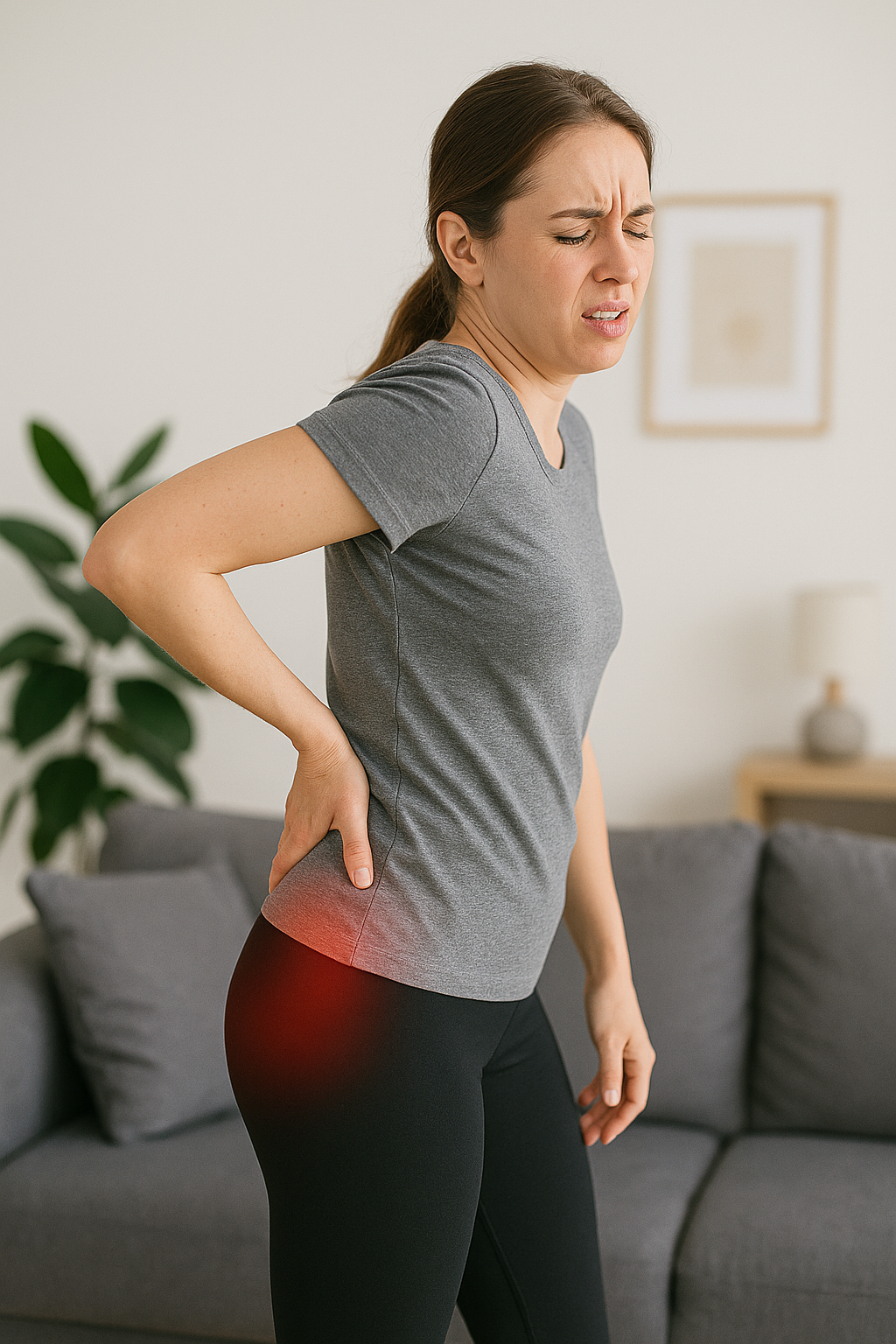
Piriformis syndrome affects millions of people each year, causing deep buttock pain that can radiate down the leg and significantly impact daily activities. Piriformis syndrome occurs when the piriformis muscle, located deep in the buttock region, becomes tight or inflamed and irritates the nearby sciatic nerve . Therapy and exercise for piriformis syndrome offers proven treatment methods to address this condition effectively, providing lasting relief and preventing future episodes through targeted exercises and manual therapy techniques. Understanding Piriformis Syndrome and Its Impact The piriformis muscle plays a crucial role in hip stability and leg rotation. This small but important muscle connects the lower spine to the upper thighbone, and the piriformis muscle helps to stabilize the hip joint during movement. When this muscle becomes tight, inflamed, or develops trigger points, it can compress the sciatic nerve that passes through the piriformis muscle, creating symptoms that mirror sciatica and contributing to what may also be classified as deep gluteal syndrome. Piriformis syndrome primarily develops from repetitive activities, prolonged sitting, or sudden increases in physical activity. Activities that cause strain on the piriformis muscle are common factors that causes piriformis syndrome. Athletes who participate in running, cycling, or sports requiring frequent direction changes face higher risk of developing this condition, often requiring specialized sports physical therapy for recovery. Office workers who spend long hours sitting also commonly experience piriformis muscle dysfunction due to sustained muscle tension and poor posture . Piriformis syndrome is characterized by several distinct symptoms that help differentiate it from other lower back pain and hip problems. The symptoms of piriformis syndrome often include deep, aching pain and discomfort in the buttock that may extend down the back of the thigh. Piriformis syndrome causes pain that typically worsens with sitting, climbing stairs, or performing activities that require hip rotation. Some individuals also experience numbness, tingling sensations, or muscle spasms that travel down the leg, similar to causes of sciatic pain , where the nerve by the piriformis muscle becomes irritated. How Physical Therapy Addresses Piriformis Syndrome Physical therapy provides comprehensive treatment options for piriformis syndrome by addressing both the immediate symptoms and underlying causes. The treatment approach for piriformis syndrome includes a multi-faceted approach that ensures patients achieve lasting relief while preventing future episodes through improved movement patterns and muscle function. The diagnosis and management of piriformis requires specialized expertise and conservative treatment methods. Pro Touch Physical Therapy employs specialized assessment techniques for accurate diagnosis of piriformis syndrome and to differentiate it from other conditions that cause similar symptoms. The evaluation process includes detailed movement analysis, muscle testing, and a piriformis stretch test that identifies piriformis muscle dysfunction and nerve irritation, helping determine whether a patient has primary piriformis syndrome. The treatment approach focuses on reducing muscle tension, improving flexibility, and strengthening supporting muscles around the piriformis muscle as well as the hip and pelvis. Manual therapy techniques, including deep tissue massage, trigger point therapy, and myofascial release , help reduce muscle tightness and trigger points within the piriformis muscle. These hands-on treatments promote blood flow, reduce inflammation, and help relax the piriformis muscle while restoring normal muscle function. Targeting the piriformis muscle through specific stretching exercises forms another essential component of treatment. Physical therapists provide guidance for progressively stretching the piriformis muscle and surrounding hip muscles. These exercises help reduce nerve compression by addressing compression of the sciatic nerve by the piriformis while improving overall hip mobility and function. Patients also learn about exercises to avoid that may worsen their condition or contribute to back pain . Specialized Treatment Techniques for Optimal Recovery Advanced physical therapy clinics utilize various specialized techniques to maximize treatment effectiveness when treating piriformis syndrome. These treatment options include dry needling, which can provide significant relief for patients with persistent muscle tension, muscle spasms, and trigger points. This treatment involves inserting thin needles into specific muscle points to release tension and reduce piriformis syndrome pain. Manual therapy techniques extend beyond basic massage to include joint mobilization and soft tissue mobilization. These specialized hands-on treatments help restore normal movement patterns and reduce muscle guarding that often accompanies piriformis syndrome. Skilled physical therapists can identify compensatory movement patterns that contribute to the condition and address these through targeted manual interventions focusing on hip muscle strengthening and movement. Heat and cold therapy applications provide additional pain relief and support the healing process. Heat therapy helps relax tight muscles and improve blood flow, while cold therapy reduces inflammation and provides pain relief during acute episodes. Physical therapists determine the optimal timing and application methods for these modalities based on each patient's specific presentation. Neuromuscular re-education plays a vital role in addressing movement dysfunction associated with piriformis syndrome. This treatment approach helps patients relearn proper movement patterns and muscle activation sequences. Through guided exercises and feedback, patients develop better body awareness and learn to move in ways that reduce stress on the piriformis muscle. Exercise Prescription and Progressive Strengthening Physical therapy exercises for piriformis syndrome include carefully prescribed exercises that progress from basic stretching to advanced strengthening activities. The exercise program as guided by the physical therapist begins with gentle stretches that can be performed multiple times daily to maintain muscle length and reduce tension. Therapy may also incorporate a seated piriformis stretch that patients can perform throughout the day to help reduce piriformis muscle tension. Hip flexor stretches help address muscle imbalances that contribute to piriformis dysfunction. Tight hip flexors can alter pelvic positioning and increase demand on the piriformis muscle. Regular stretching of these muscles helps restore proper hip mechanics and reduces piriformis strain, with exercises help improve muscle flexibility and function. Glute strengthening exercises play a crucial role in piriformis syndrome recovery, particularly for an individual with piriformis syndrome focusing on long-term prevention. Weak gluteal muscles often contribute to piriformis overactivity as this smaller muscle compensates for inadequate support from larger muscle groups. Targeted strengthening exercises help restore proper muscle balance and reduce excessive demand on the piriformis muscle, with syndrome focusing on hip muscle development being essential for recovery. Core stabilization exercises support overall pelvic stability and reduce compensatory patterns that strain the piriformis muscle. A strong core provides a stable foundation for hip movement and helps maintain proper posture during daily activities. Physical therapists prescribe progressive core exercises that challenge stability while maintaining proper form, and patients must comply with the exercise program for optimal results. Functional movement training helps patients apply their improved strength and flexibility to real-world activities, representing the best piriformis syndrome rehabilitation approach. This training includes practicing movements like walking, climbing stairs, and getting in and out of chairs with proper mechanics. Physical therapy may also incorporate aerobic exercise to improve overall conditioning while supporting recovery. Functional training ensures that improvements gained through therapy translate to better performance in daily activities and helps prevent piriformis syndrome recurrence. Advanced Treatment Approaches and Technology Modern physical therapy clinics incorporate advanced technologies and treatment approaches to enhance piriformis syndrome recovery. Treatment of an individual with this condition may include ultrasound therapy that uses sound waves to promote deep tissue healing and reduce inflammation around the piriformis muscle. This non-invasive treatment penetrates deep into the muscle tissue, providing therapeutic benefits that complement manual therapy techniques targeting areas underneath the piriformis. Electrical stimulation therapy can help reduce pain and promote muscle relaxation in patients with piriformis syndrome. This treatment uses controlled electrical impulses to stimulate nerve pathways and reduce pain signals. Some patients find electrical stimulation particularly helpful for managing pain during the initial phases of treatment, and the approach for piriformis syndrome includes various types of piriformis muscle treatments. Movement analysis technology allows physical therapists to identify subtle movement patterns that contribute to piriformis syndrome. High-tech assessment tools can detect compensatory movements and muscle activation patterns that may not be visible during standard evaluation. This information guides treatment planning and helps ensure comprehensive correction of movement dysfunction, with piriformis syndrome includes a focus on detailed biomechanical analysis. Pro Touch Physical Therapy utilizes cutting-edge treatment technologies that accelerate recovery and maximize treatment outcomes. Their advanced equipment and specialized techniques provide patients with access to the most effective piriformis syndrome treatments available, with interventions focusing on hip muscle strengthening as a core component of care. Recovery Timeline and Long-Term Management Piriformis syndrome recovery timeline varies based on symptom severity, contributing factors, and individual patient characteristics. Most patients begin experiencing symptom improvement within the first few weeks of consistent physical therapy treatment. However, complete recovery typically requires several months of dedicated therapy and home exercise compliance, with piriformis syndrome aim focused on achieving lasting results. Early recovery focuses on pain reduction and muscle relaxation through manual therapy and gentle stretching. Patients often notice decreased buttock pain and improved comfort with sitting during this initial phase. As symptoms improve, treatment progresses to include strengthening exercises and movement retraining, with interventions designed to help reduce piriformis muscle tension and inflammation. The intermediate recovery phase emphasizes restoring normal muscle function and movement patterns. Patients work on more challenging exercises that prepare them for return to full activity levels. This phase typically includes progressive strengthening and functional movement training. Long-term management involves maintaining the gains achieved through physical therapy and preventing future episodes. The management of piriformis syndrome requires patients to learn home exercise programs that help maintain muscle flexibility and strength, and piriformis and surrounding muscle groups require ongoing attention. Regular exercise and proper movement mechanics become essential components of ongoing piriformis syndrome management, working to prevent the recurrence of piriformis syndrome symptoms through consistent self-care practices that help relieve piriformis syndrome symptoms. Preventing Future Episodes Through Education Education plays a vital role in piriformis syndrome treatment success and prevention of future episodes. Physical therapists teach patients about factors that contribute to their condition and strategies for avoiding symptom recurrence. The piriformis muscle and sciatic nerve relationship requires careful attention to movement patterns and activity modifications. Workplace ergonomics education helps office workers modify their work environment to reduce piriformis strain and prevent associated back pain. This includes proper chair height, sitting posture, and regular movement breaks that prevent prolonged muscle tension. Simple workplace modifications can significantly reduce the risk of piriformis syndrome recurrence. Activity modification guidance helps athletes and active individuals continue participating in their chosen activities while protecting the piriformis muscle. This may include warm-up strategies, training progression guidelines, and technique modifications that reduce injury risk and prevent back pain related to piriformis dysfunction. Home exercise program instruction ensures patients can continue their recovery progress between physical therapy sessions. Patients learn proper exercise technique and progression guidelines that support continued improvement. Consistent home exercise compliance directly correlates with better treatment outcomes and reduced recurrence of piriformis syndrome. Experience Personalized Piriformis Syndrome Recovery at Pro Touch Physical Therapy Effective treatment of piriformis syndrome requires specialized knowledge, individualized care, and comprehensive treatment approaches that address both symptoms and underlying causes. The complex nature of this condition demands expertise in manual therapy, exercise prescription, and movement analysis to achieve optimal outcomes. Diagnosis and management of piriformis syndrome should be handled by qualified professionals who understand the relationship between piriformis dysfunction and associated back pain symptoms. Patients who experience persistent buttock pain and leg symptoms should seek evaluation from qualified physical therapy professionals who can provide accurate diagnosis and effective treatment strategies. Pro Touch Physical Therapy offers specialized piriformis syndrome treatment through personalized, one-on-one care that addresses your unique needs and recovery goals. Their experienced therapists combine advanced manual therapy techniques with evidence-based exercise programs to help you achieve lasting relief from piriformis syndrome symptoms. Contact Pro Touch Physical Therapy today at (908) 325-6556 to schedule your comprehensive evaluation and begin your path to recovery from piriformis syndrome .